Introduction
The Durable Medical Equipment (DME) billing process is a complex journey that requires attention to detail, adherence to regulations, and effective communication between multiple parties. This comprehensive guide will walk you through each step of the process, from the initial prescription to the final payment, providing insights, best practices, and expert tips along the way.
Prescription and Medical Necessity
The DME billing process begins with a prescription from a qualified healthcare provider. This step is crucial as it establishes medical necessity, a key requirement for insurance coverage and reimbursement.
Key Components:
- Detailed written order (DWO)
- Patient’s diagnosis
- Length of need
- Provider’s signature and date
Best Practices:
- Use electronic prescribing systems to reduce errors and improve efficiency
- Implement a checklist system to verify all required elements are included
- Maintain open lines of communication with prescribing physicians
Patient Intake and Insurance Verification
Once a prescription is received, the next step is to gather patient information and verify insurance coverage.
Patient Intake:
- Collect demographic information
- Obtain signed consent forms
- Educate patient on equipment use and billing process
Insurance Verification:
- Check coverage for specific DME items
- Verify policy limits and restrictions
- Determine if prior authorization is required
Best Practices:
- Use automated insurance verification tools to streamline the process
- Document all communication with insurance companies
- Train staff on how to explain benefits and potential out-of-pocket costs to patients
Prior Authorization
Many DME items, especially high-cost equipment, require prior authorization from the insurance company.
Steps in Prior Authorization:
- Gather required documentation (prescription, medical records, etc.)
- Submit authorization request to the insurer
- Follow up on pending authorizations
- Document approval or denial
Common Challenges:
- Incomplete documentation
- Delayed responses from insurers
- Denials due to lack of medical necessity
Best Practices:
- Develop a tracking system for authorization requests
- Create templates for common authorization requests to ensure consistency
- Establish a process for appealing denials
Equipment Delivery and Set-up
Once authorization is obtained, the DME can be delivered to the patient.
Key Considerations:
- Coordinate delivery time with the patient
- Ensure proper set-up and patient education
- Obtain signed proof of delivery (POD)
Best Practices:
- Use mobile technology for real-time delivery updates and electronic signatures
- Provide patients with written instructions and contact information for support
- Implement a follow-up process to ensure patient satisfaction and address any issues
Claim Preparation and Submission
With delivery confirmed, the next step is to prepare and submit the claim.
Essential Elements of a DME Claim:
- Patient information
- Insurance details
- Appropriate HCPCS codes and modifiers
- Date of service
- Charge amount
Claim Submission Methods:
- Electronic claims (recommended for faster processing)
- Paper claims (CMS-1500 form for most insurers)
Best Practices:
- Implement claim scrubbing software to catch errors before submission
- Establish a quality control process to review claims before submission
- Stay updated on payer-specific requirements and deadlines
Payment Posting and Account Reconciliation
Once claims are processed, payments (or denials) will be received from the insurer.
Payment Posting Process:
- Receive and review Explanation of Benefits (EOB) or Electronic Remittance Advice (ERA)
- Post payments to patient accounts
- Identify any discrepancies or underpayments
Account Reconciliation:
- Compare expected reimbursement to actual payment
- Identify and address any discrepancies
- Update patient accounts for any remaining balance
Best Practices:
- Use automated posting systems for accuracy and efficiency
- Regularly audit posted payments to ensure accuracy
- Develop a process for addressing underpayments or incorrect denials
Follow-up on Unpaid Claims and Denials
Not all claims will be paid on the first submission. A robust follow-up process is crucial for maximizing reimbursement.
Follow-up Steps:
- Identify unpaid or denied claims
- Determine reason for non-payment (e.g., missing information, coding errors, lack of medical necessity)
- Correct and resubmit claims or file appeals as necessary
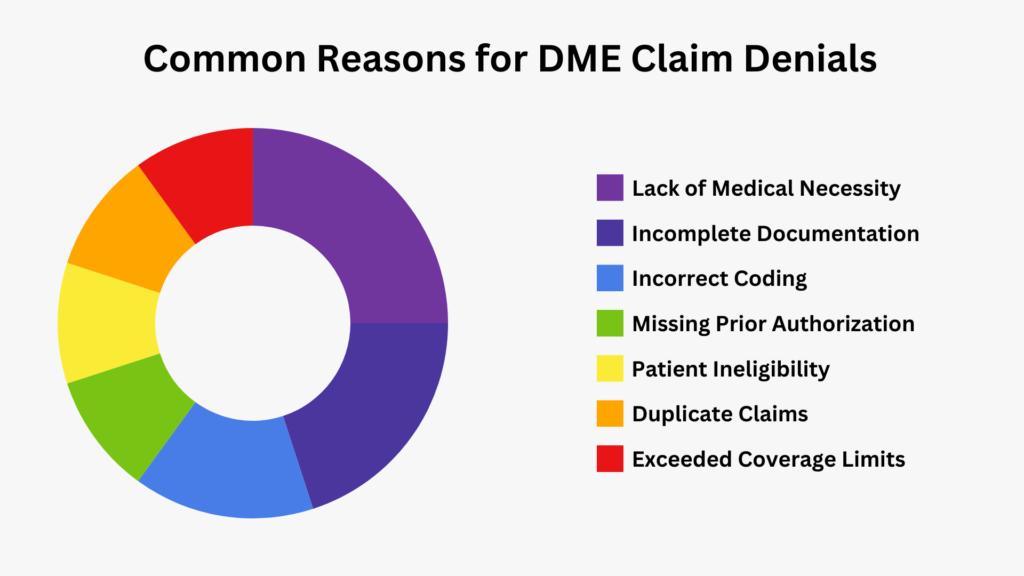
Common Reasons for Denials:
- Incorrect or missing patient information
- Invalid or expired insurance
- Lack of prior authorization
- Incorrect coding or modifiers
Best Practices:
- Establish a timeline for following up on unpaid claims (e.g., 30, 60, 90 days)
- Develop a denial management system to track and address each denial
- Analyze denial patterns to identify and address recurring issues
Ongoing Maintenance and Rental Billing
For rental equipment or supplies that require regular refills, billing is an ongoing process.
Rental Billing Considerations:
- Track rental periods and cap limits
- Monitor changes in medical necessity
- Handle upgrades or changes in equipment
Supply Refill Process:
- Establish a schedule for contacting patients about refills
- Verify continued need and usage of supplies
- Update prescriptions as necessary
Best Practices:
- Implement an automated system for tracking rental periods and initiating refill contacts
- Regularly communicate with patients and providers to ensure continued medical necessity
- Stay informed about changes in coverage policies for long-term rentals and supplies
Compliance and Auditing
Maintaining compliance with healthcare regulations and payer policies is crucial in DME billing.
Key Compliance Areas:
- Documentation requirements
- Coding accuracy
- Privacy and security (HIPAA compliance)
- Fraud, waste, and abuse prevention
Auditing Process:
- Conduct regular internal audits
- Review claims for accuracy and completeness
- Verify proper documentation for all billed items
- Address any identified issues promptly
Best Practices:
- Develop a compliance plan specific to DME billing
- Provide ongoing staff training on compliance issues
- Stay updated on changing regulations and payer policies
- Consider engaging external auditors periodically for an objective review
The DME billing process is complex and requires attention to detail at every step. By understanding each phase of the process and implementing best practices, DME suppliers and billing professionals can improve efficiency, reduce denials, and ultimately provide better service to patients.
Remember, successful DME billing is not just about getting paid—it’s about ensuring patients have access to the medical equipment they need while maintaining compliance with healthcare regulations and payer policies.
How WWS Can Help Streamline Your DME Billing Process
While understanding the DME billing process is crucial, implementing and maintaining an efficient system can be challenging. This is where Worldwide Solutions Health Care Services (WWS) comes in. We specialize in optimizing DME billing processes for healthcare providers and suppliers.
Our Expertise
- In-depth knowledge of DME billing regulations and best practices
- Experience with various DME billing software and systems
- Skilled team of billing specialists and compliance experts
WWS Services for DME Billing
- Process Optimization: We analyze your current billing process and implement improvements to increase efficiency and accuracy.
- Compliance Assurance: Our team ensures your billing practices meet all regulatory requirements, reducing the risk of audits and penalties.
- Staff Training: We provide comprehensive training to your team, keeping them updated on the latest DME billing practices and regulations.
- Denial Management: Our experts help reduce claim denials and efficiently handle appeals when necessary.
- Technology Integration: We assist in selecting and implementing the right DME billing software for your needs.
Take the Next Step
Ready to optimize your DME billing process? WWS offers a Collaborative Discovery Meeting to discuss your specific needs and how we can help.
Schedule Your WWS Collaborative Discovery Meeting Today: https://calendly.com/wwshcs/wws-collaborative-discovery-meeting
During this meeting, we’ll:
- Assess your current DME billing challenges
- Discuss potential solutions tailored to your organization
- Provide insights on how WWS can support your DME billing goals
- Answer any questions you have about our services and approach
Don’t let DME billing complexities hold your organization back. Partner with WWS for expert support and guidance.
External Links:
- CMS Durable Medical Equipment Center – https://www.cms.gov/Center/Provider-Type/Durable-Medical-Equipment-DME-Center
- AAFP: Durable Medical Equipment: A Guide to Billing Medicare – https://www.aafp.org/pubs/fpm/issues/2022/0300/p23.html